What You Should Know Before Joint Replacement Surgery
Being Prepared Is the First Step Toward a Successful Surgery
Hip and knee replacement surgeries are among the most effective treatments for patients with advanced joint degeneration and chronic pain that limits daily function. While these procedures significantly improve quality of life, they are not routine interventions—they require careful planning before, during, and after the operation.
In this article, we’ll guide you through everything you need to know before joint replacement surgery, from medical and physical preparations to postoperative expectations and mental readiness.
1. When Is Joint Replacement Surgery Recommended?
Your orthopedic surgeon may recommend a joint replacement when:
- Non-surgical treatments (medications, injections, physical therapy) fail
- Pain significantly interferes with walking, climbing stairs, or daily activities
- You experience nighttime pain and poor sleep
- Imaging shows severe joint space narrowing or bone-on-bone contact
- Your overall quality of life is noticeably reduced
Surgical decisions are based on clinical findings, patient history, X-rays, and MRI results.
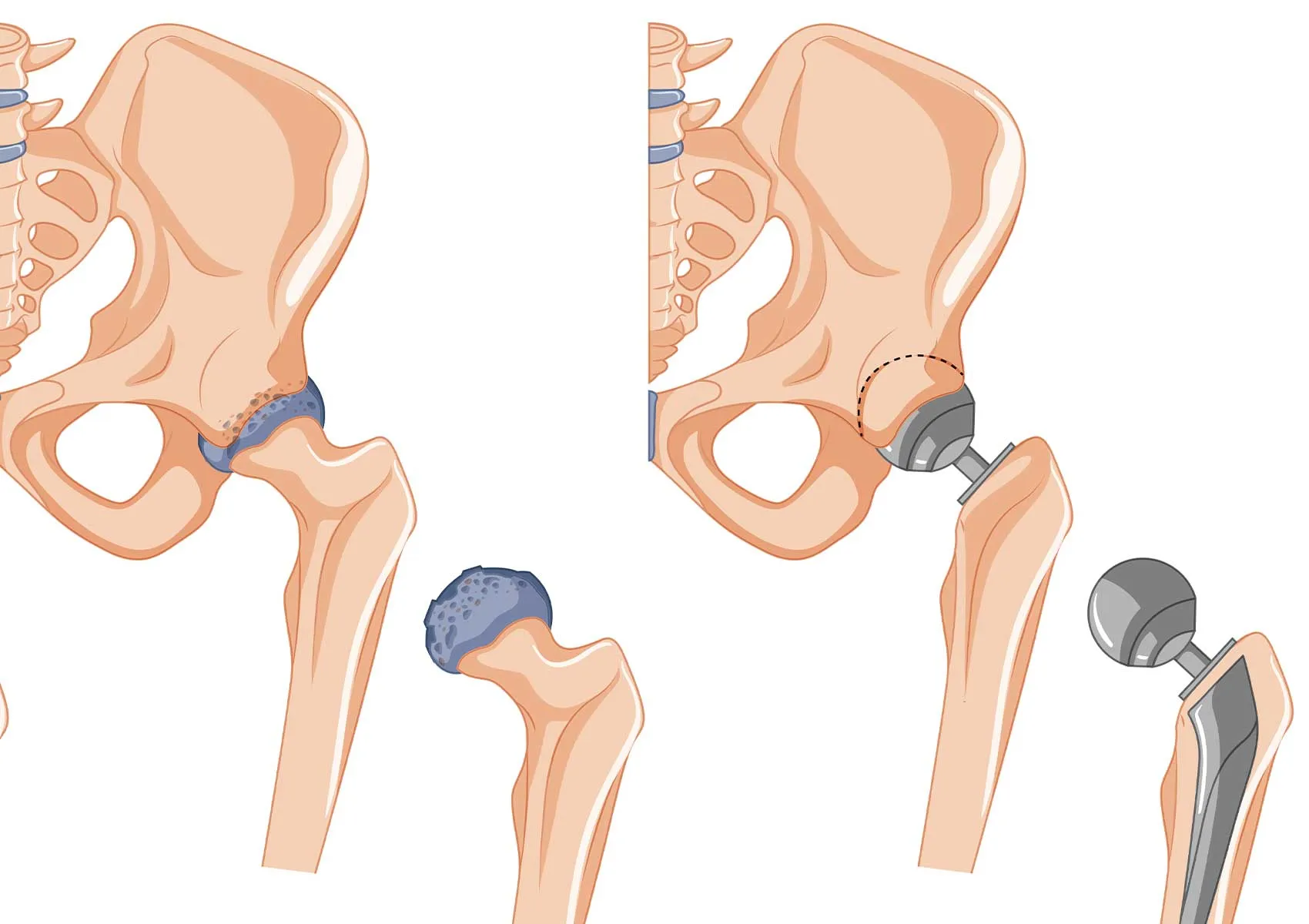
2. What Type of Prosthesis Will Be Used?
There are different types of joint prostheses depending on the joint and condition:
- Total joint replacement – replacing all joint surfaces
- Partial (unicompartmental) replacement – replacing only one part of the joint
- Cemented or cementless fixation
- Components made of metal, ceramic, or polyethylene
Your surgeon will choose the best option based on your age, bone quality, activity level, and overall health.
3. How to Prepare Before Surgery
Medical Preparation:
- Blood tests, EKG, and chest X-ray will be performed
- A pre-anesthesia consultation is required
- Chronic conditions (diabetes, hypertension, cardiac issues) should be stabilized
- Any existing infections, including dental or gum issues, must be treated
Physical Preparation:
- Begin light preoperative exercises to strengthen leg muscles
- Prepare your home for safety: remove tripping hazards, install grab bars if needed
- Get assistive devices like crutches or a walker in advance
Psychological Preparation:
- Learn about the procedure and set realistic expectations
- Understand that recovery takes time, effort, and patience
- Communicate with family or caregivers for emotional and practical support
Being well-prepared improves confidence and contributes to better recovery outcomes.
4. How Long Will You Stay in the Hospital?
Most joint replacement patients stay in the hospital for 2 to 4 days, depending on the type of surgery and recovery speed. During this time:
- Pain control is initiated
- You will begin walking with assistance
- Physical therapy is introduced early for better outcomes
Some hospitals follow enhanced recovery protocols, allowing same-day mobilization and even shorter stays.
5. What Happens After Surgery?
- Day 1: You will likely stand and begin walking with support
- Week 1: Dressings are checked, pain medications are continued
- Week 2–4: Sutures are removed, and structured physical therapy begins
- Month 1–3: You return to most daily activities
- After Month 6: Gradual return to hobbies and light sport is possible
Remember, surgery alone doesn’t guarantee success—adherence to rehabilitation and guided exercises is crucial for optimal recovery.
6. Set Realistic Expectations
Joint replacement is highly effective, but it's important to approach the process with balanced expectations:
- Your new joint may not feel exactly like a natural joint
- High-impact sports and deep squatting are generally discouraged
- Implants have a limited lifespan (typically 15–20 years)
- Minor stiffness or occasional soreness may persist in some cases
Open communication with your surgeon and understanding what to expect can lead to higher satisfaction.
FAQ
-
Will I be in pain after surgery?
Yes, but modern pain management protocols make it manageable and often well-controlled within a few days.
-
Is there a best season for joint replacement?
There’s no ideal season—your health and preparation are far more important than the time of year.
-
Is joint replacement high risk?
Like any surgery, there are risks. But with proper planning and a skilled team, success rates are very high.
-
How long does a joint prosthesis last?
Typically 15–20 years, depending on your activity level, weight, and implant type.
-
Is it normal to feel nervous before surgery?
Yes. It’s perfectly natural. Learning about the procedure and asking questions can reduce anxiety and help you feel more in control.