- Mon - Sat: 9:00
- Call Us: +90 (538) 894 00 91
- [email protected]
Hip Joint Diseases
The hip joint is a ball-and-socket joint composed of the femoral head and the acetabulum. Painless movement in the joint is facilitated by the hyaline cartilage covering the joint surfaces. The hip joint capsule is a thick and strong structure that significantly contributes to the stability of the joint.
The labrum is a fibrocartilage structure that lines the rim of the acetabulum, increasing the depth of the joint and contributing to joint stability. The labrum provides a seal-like function in the joint, ensuring that synovial fluid remains in the central joint space and aiding in the survival of articular cartilage. Damage to this structure can lead to complaints such as pain, catching, and locking in the joint.
Labral tears predominantly occur in the presence of underlying bony abnormalities such as femoroacetabular impingement or acetabular dysplasia. Additionally, they can occur traumatically in athletes with hypermobility or individuals with joint laxity.
Factors causing labral tears:
Labral tears most commonly present with groin pain. Patients often describe a deep and sharp pain. The pain typically increases with activity. Activities requiring hip flexion and internal rotation, such as sitting in low positions or getting in and out of a car, tend to provoke symptoms. Rarely, patients may also experience pain in the back or lateral aspect of the hip.
The labrum tissue contains numerous free nerve endings, which is why labral tears can result in a highly painful clinical condition.
In the treatment of labral tears, aside from addressing the underlying bony problem, partial debridement of the labrum (removal of torn parts), labral repair, or labral reconstruction may be performed. The treatment decision is based on factors such as the location of the torn labral tissue, its chronicity (whether the tear is recent or old), and the tissue quality.
If the labral tissue quality is compromised (e.g., worn or calcified tissue), labral debridement may be performed. Specialized shavers and radiofrequency probes are used to remove the damaged area from the joint.
If the labral tissue quality is sufficient for healing, labral repair can be performed using bone anchor sutures placed along the acetabular rim. The bone anchors used in this repair are absorbable and dissolve within the bone after labral healing.
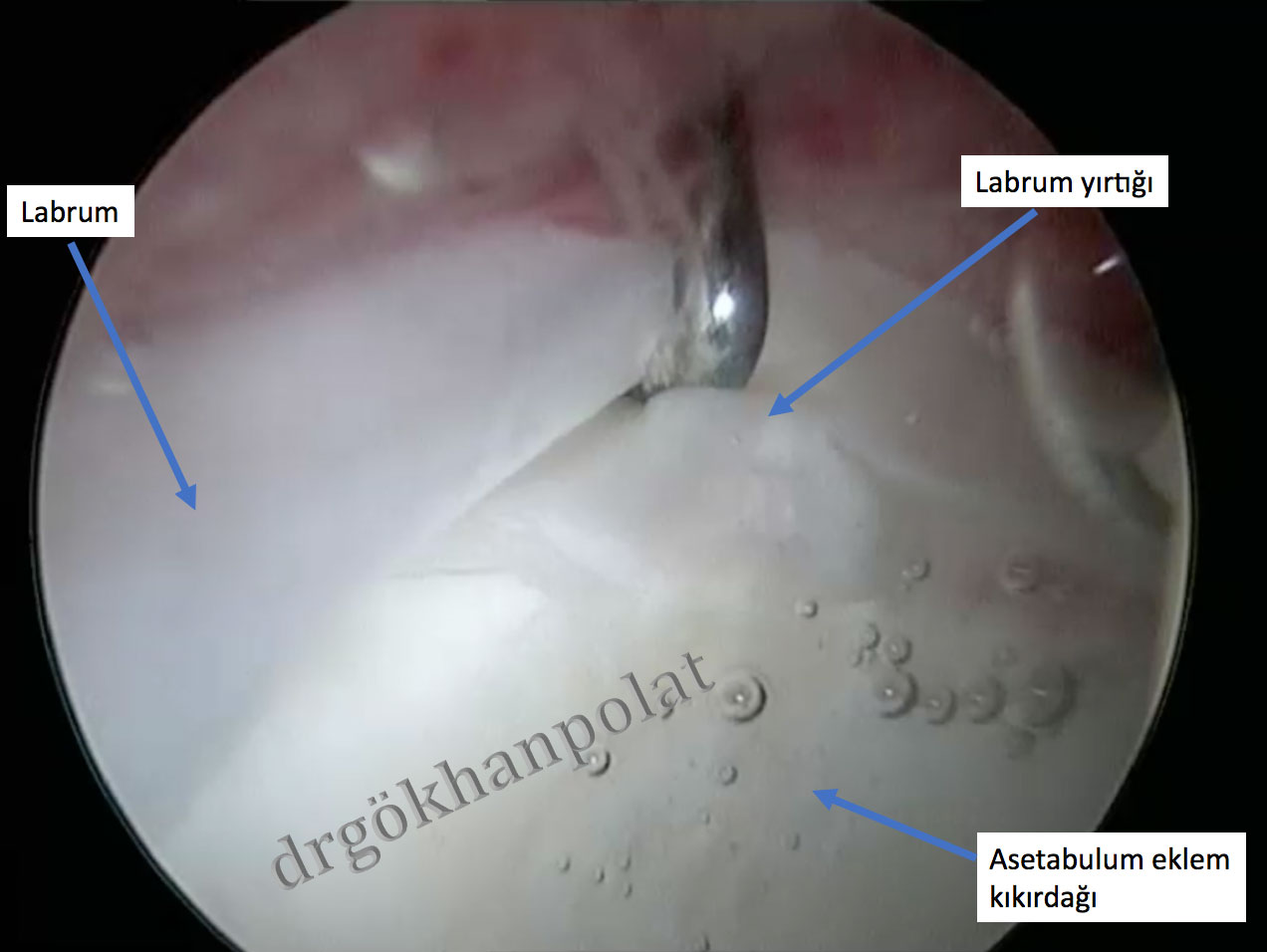
Figure: Appearance of the hip joint and labral tear during arthroscopy
In cases of previously failed surgical treatments or degenerative labral tears (worn and biomechanically compromised) that cannot be repaired, labral reconstruction may be performed during revision hip arthroscopy. Reconstruction can be performed using tissue harvested from another part of the body or an allograft (gracilis tendon from a cadaver).
Due to morphological abnormalities in the hip joint, it is the pathological contact and impingement that develops between the femoral head-neck junction and the acetabulum. Three types of femoroacetabular impingement have been described: CAM type, Pincer type, and Combined type.
Secondary damage within the joint (labral tears and cartilage damage) caused by impingement can lead to a clinical condition causing hip pain in patients. This clinical condition is referred to as femoroacetabular impingement syndrome. The pathophysiological process developing within the joint due to impingement is considered a risk factor for hip osteoarthritis (joint degeneration) in the long term.
CAM type impingement is caused by the femur. Typically, there is a bony prominence (CAM lesion) on the anterolateral (front-side) aspect of the femoral neck. This causes a shearing force within the joint as the femoral head enters the acetabulum. This impingement leads to extensive labral tears and cartilage damage. It is more commonly seen in young male patients. (Figure 1)
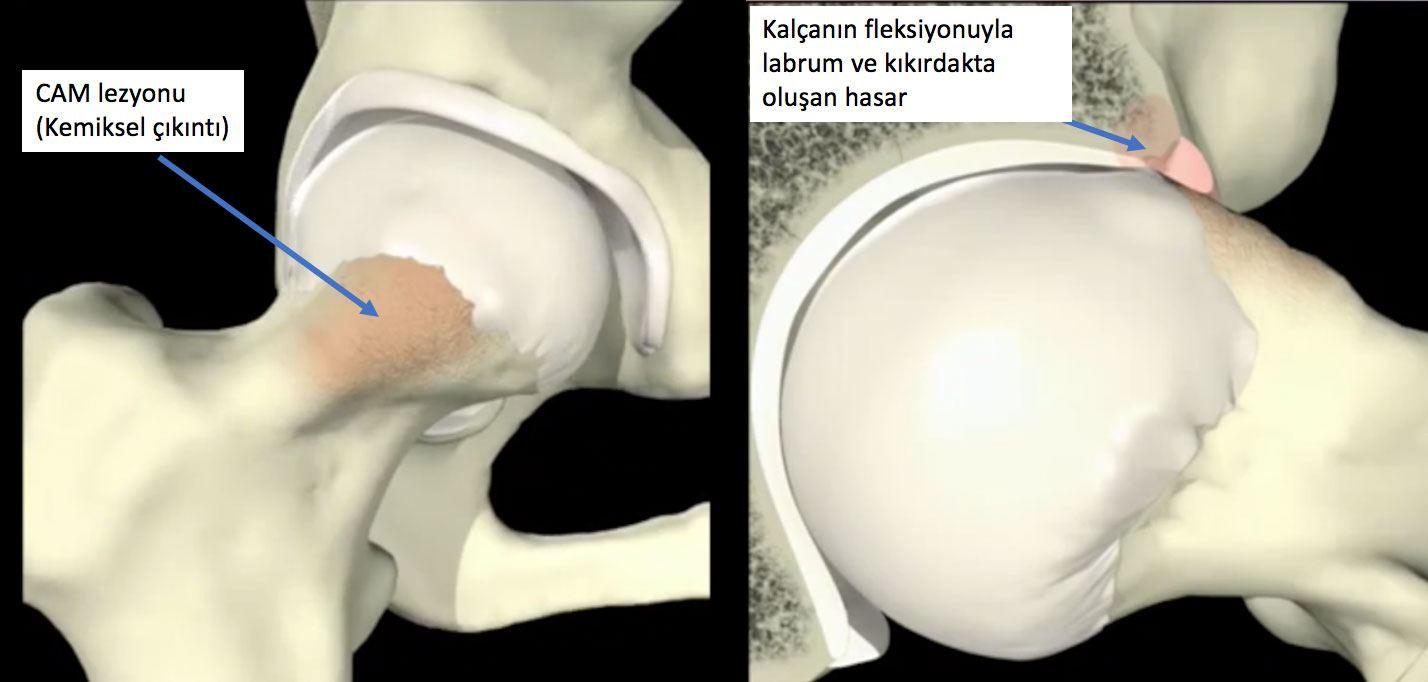
Figure 1: The bony abnormality causing CAM type impingement and the damage occurring during joint movement are shown.
It develops due to excessive coverage of the acetabulum. It is more commonly seen in middle-aged female patients. Secondary damage in the joint develops more slowly compared to CAM type. (Figure 2)
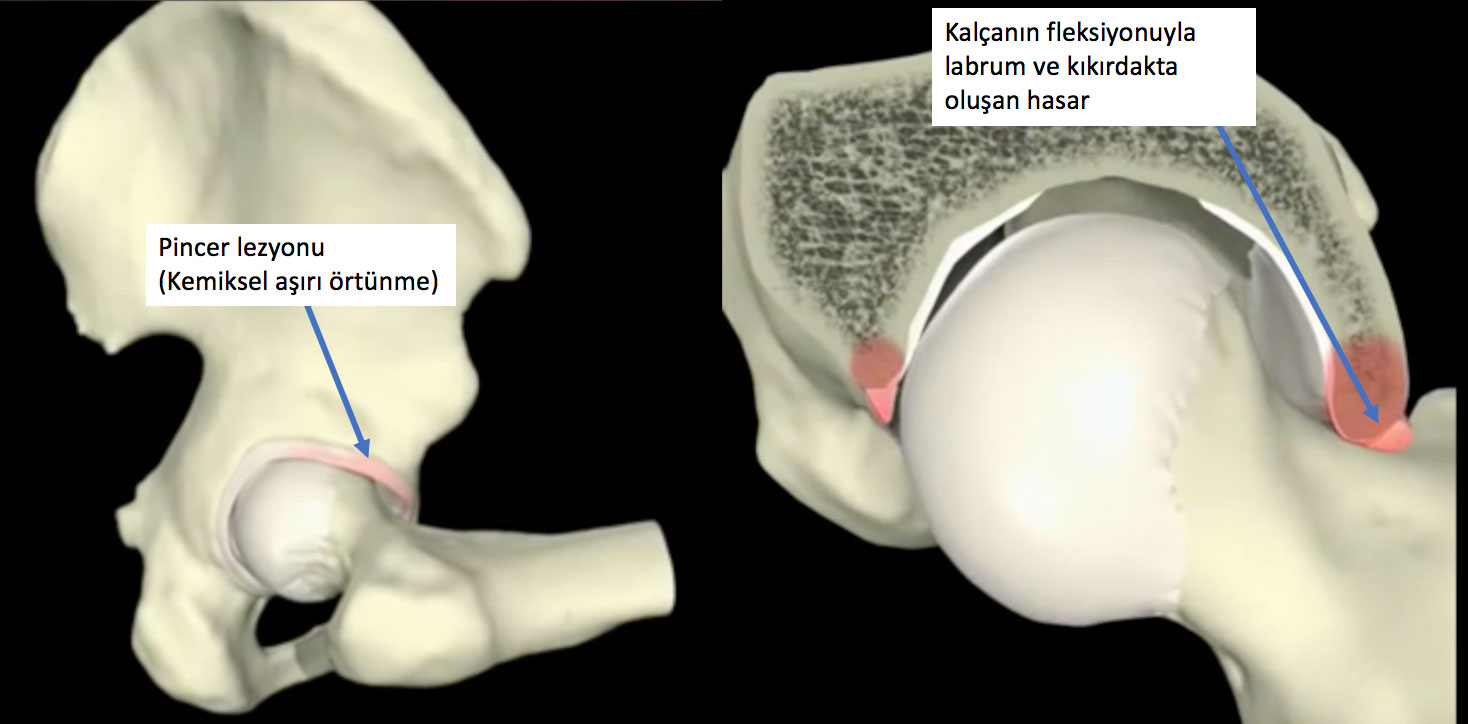
Figure 2: The bony abnormality causing Pincer type impingement and the damage occurring during joint movement are shown.
This is the type where both impingement types are seen together. It is the most commonly encountered type of impingement.
Patients experience restricted hip movement and pain due to bony deformities and clinical symptoms. Typically, patients have groin pain radiating to the lateral hip, triggered by activity. The pain can be dull or sharp in character. Complaints often increase with activities such as sitting and standing.
Athletes (e.g., football players, bodybuilders), individuals carrying heavy loads, and those with a history of hip joint disease during childhood are more frequently affected.
The diagnosis can be made through X-ray examinations following an evaluation by an experienced orthopedist. Magnetic resonance imaging (MRI) is highly useful for visualizing secondary damage in the joint.
In individuals where non-surgical treatment fails, surgical treatment should be applied. Femoroacetabular impingement is the most common clinical condition for which hip arthroscopy is used today. Through treatment applied via 3-4 portals (entry points), in addition to repairing damaged structures within the joint, it is possible to fully arthroscopically address the Pincer lesion (shaving of the acetabulum, acetabuloplasty) and the CAM lesion (shaving of the femoral head-neck junction, femoroplasty) causing impingement. (Figures 3-4) In experienced hands, clinical success rates after arthroscopic treatment of patients are in the 90% range for 2-5 years.

Figure 3: Hip arthroscopy
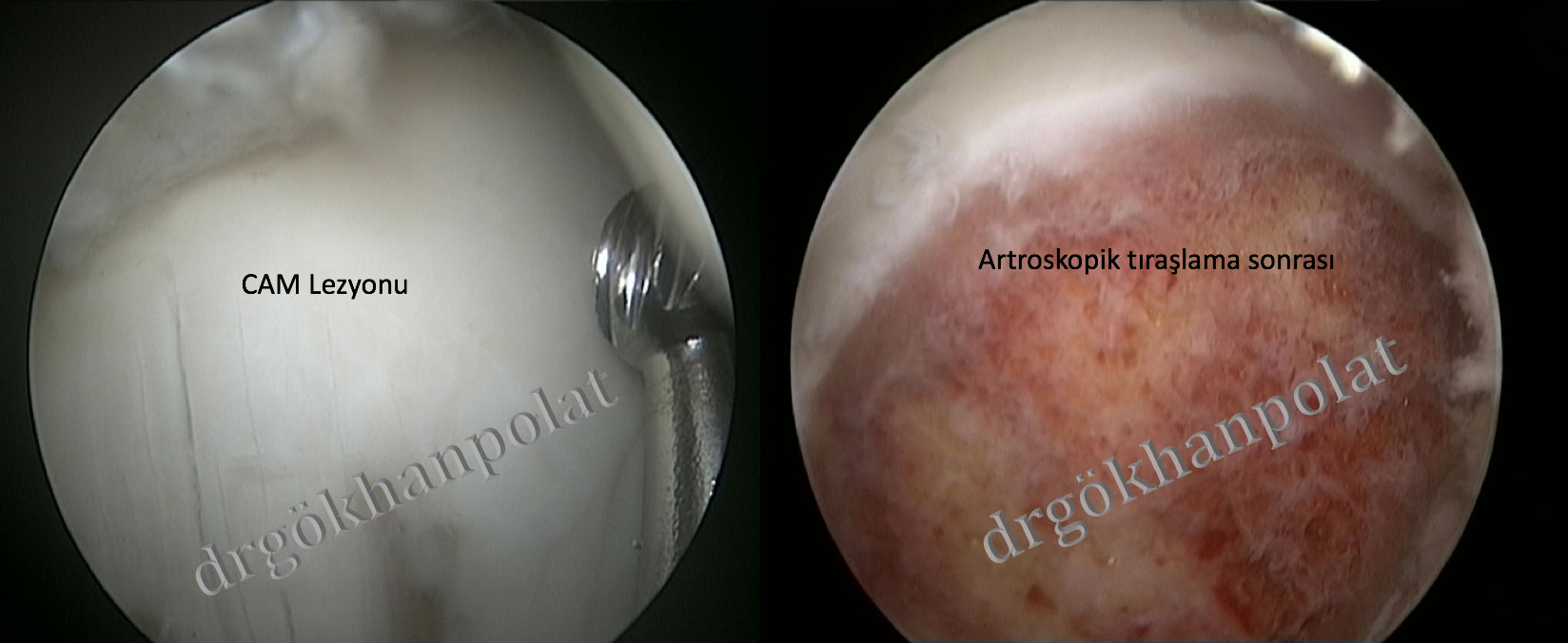
Figure 4: Treatment of the CAM lesion with hip arthroscopy
This is a pathology where the anterior inferior iliac spine forms a protrusion toward the hip joint due to developmental or traumatic causes, leading to impingement in the anterior part of the hip. It may occur concurrently with femoroacetabular impingement. In symptomatic patients, the bony morphological abnormality can be addressed endoscopically or through open surgery.
This is the pathological contact and impingement that develops between the ischium and the lesser trochanter. It is typically seen in middle-aged female patients. Medications, activity modification, physical therapy exercises, and injections can yield satisfactory results in treatment. Surgical treatments may be applied in patients where these approaches fail.
Cartilage tissue is a flexible and slippery connective tissue. It covers joint surfaces, reduces friction in the joint, and aids in shock absorption. Healthy articular cartilage is essential for painless joint movement.
Cartilage lesions are common. However, due to the lack of its own blood supply, the likelihood of healing after injury is quite limited.
Treatment of cartilage lesions in the hip joint can be similar to that of other joints. In cases of significant cartilage damage, surgical treatment may be necessary. Arthroscopic lavage, debridement, bone marrow stimulation, mosaicplasty, autologous osteochondral graft transfer, and autologous chondrocyte implantation can be performed.
Adductor tendon injuries are common in athletes in the hip region. This condition, which causes groin pain, develops due to damage at the insertion site of the adductor magnus, longus, medius, and gracilis muscles on the inner thigh. Tears typically occur at the muscle-tendon junction. Injuries in this region can vary in severity, including mild injury (Stage 1), moderate injury (Stage 2 partial tear), and full-thickness injury (Stage 3 complete tear).
Injuries often occur due to sudden contractions (e.g., kicking a ball, sudden turns). Inadequate warm-up, stretching exercises, or muscle fatigue from overuse commonly contribute to the injury.
The injury is characterized by a sudden onset of pain in the inner groin region, often accompanied by a tearing sound. Diagnosis is typically confirmed through physical examination. In professional athletes, MRI is used to stage the injury and provide detailed information about the athlete’s return to sports.
In the vast majority of athletes, conservative (non-surgical) treatments are sufficient. With specialized rehabilitation programs, athletes can return to sports after the third week. Surgical treatments may be applied in cases of recurrent injuries or when conservative treatment fails.
The hamstring muscles, located at the back of the inner thigh, are frequently injured due to their crossing of both the knee and hip joints. These injuries are common in sports such as football and basketball, which require sudden acceleration and direction changes.
The proximal hamstring tendons (semitendinosus, semimembranosus, and biceps femoris) attach to the pelvic bone at the back of the hip joint. Depending on the severity of the sports injury, damage ranging from simple strains to full-thickness tears can occur in these structures. Additionally, sudden contractions of these tendons can sometimes cause an avulsion fracture (bone fragment detachment) at their attachment site on the pelvic bone.
Injuries typically occur following sudden and forceful muscle contractions, such as during jumping, sudden stopping, or excessive stretching. At the time of injury, patients experience severe pain and muscle weakness. Physical examination reveals tenderness, swelling, and bruising at the back of the hip and upper thigh. Diagnosis is easily confirmed with X-rays and MRI scans.
Treatment decisions are based on factors such as the level of athletic activity, the number of injured tendons, and their location. In conservative (non-surgical) treatment, rest, medications, PRP injections, and physical therapy and rehabilitation exercises in the later stages of healing are highly beneficial. Surgical treatment involves reattaching the bone fragment detached with the tendon to the bone or reattaching tendons torn near the bone to the bone using anchor sutures. After surgical treatment, the use of crutches and a brace for a period is necessary to protect the repaired area.
The gluteus medius is one of the three large muscles located at the side and back of the hip region. Its primary function is to contribute to pelvic stability and enable lateral movement of the hip joint.
This tendon is subjected to significant loads during certain hip movements. As a result, it can be damaged due to trauma or degenerative processes, leading to hip pain and weakness in patients.
In patients diagnosed with partial tears or tendinopathy (a chronic condition where the tendon’s biological integrity is compromised), initial treatment includes ice application, anti-inflammatory medications, and avoiding activities that strain the tendon. In patients whose symptoms persist despite physical therapy and rehabilitation, surgical treatments such as arthroscopic or open repair may be necessary.
Snapping hip is characterized by a snapping sensation and sound around the hip during movements such as standing up from a chair, walking, or running, when the legs are in motion. It occurs due to the snapping of muscles and tendons over bony prominences around the hip. It can be observed in approximately 20% of the general population asymptomatically (harmless and painless). This condition can sometimes lead to bursitis, a painful clinical condition around the hip.
Treatment includes non-surgical interventions such as activity modification, ice application, and medications. Physical therapy and rehabilitation exercises focusing on stretching and flexibility of the structures causing the snapping are essential. Depending on the level of pain, corticosteroid injections may be applied to the bursitis-affected area.
In patients where non-surgical treatment options fail, the pathology causing this condition can be addressed with open or arthroscopic treatments.
Hip joint stability is critically important for movements such as standing, walking, and running, which require support of the body. The bony structure of the hip joint primarily provides this stability. Additionally, the labrum, ligamentum teres, and hip joint capsule are other important structures involved in this stability. Congenital, developmental, or traumatic conditions affecting these structures can lead to hip joint instability.
Patients may experience symptoms such as pain, laxity (looseness), a sensation of the hip giving way, or sounds coming from the hip.
This instability may develop due to congenital causes (e.g., developmental hip dysplasia), developmental conditions (e.g., pediatric diseases like slipped capital femoral epiphysis), or traumatic injuries (e.g., sports injuries, traffic accidents). Common causes include labral or ligament injuries, hip dysplasia (inadequate bony coverage), femoroacetabular impingement (bony mismatch), and ligamentum teres tears.
The diagnosis of this condition, which causes hip pain, can be made through detailed examination and diagnostic tests.
Athletic pubalgia, also known as sports hernia, is a clinical condition that causes groin pain. It can develop during sports activities involving sudden turns or direction changes. This clinical condition, which occurs due to damage to structures in the inner abdominal wall that attach to the pelvis, can be confused with many other pathologies due to groin pain.
The pain typically resolves with rest but recurs with activity and sports. A resisted sit-up test often elicits significant pain in the groin area. Treatment with core-strengthening exercises, rehabilitation, and temporary cessation of sports can yield satisfactory results. In patients who do not respond to these treatments, laparoscopic or open surgical treatments can be performed.
Osteitis pubis is a clinical condition that develops in athletes due to overuse. This condition, which presents with groin pain, occurs due to inflammation caused by excessive mechanical forces on the pubic bones and the symphysis pubis region at the front of the pelvis.
Pain is triggered by contraction of the hip adductors and flexors. Coughing or sneezing can cause sharp pain.
Rehabilitation is achieved with core-strengthening exercises to balance lumbopelvic control, and cessation of sports is necessary. Surgical treatment should be applied in athletes with persistent symptoms.
Piriformis syndrome is a rare neuromuscular condition caused by the piriformis muscle compressing the sciatic nerve.
It typically causes pain and numbness-like symptoms at the back of the hip. Activities that increase the compression of the sciatic nerve by the piriformis, such as driving or running, exacerbate symptoms.
Treatment includes activity modification, stretching exercises, and medical therapies. In patients whose symptoms persist despite these treatments, decompression treatments targeting the sciatic nerve may be necessary.