Infection Risk After Joint Replacement
Learn about infection risk after joint replacement surgery. Discover warning signs, treatment strategies, and prevention tips to protect your implant and health.
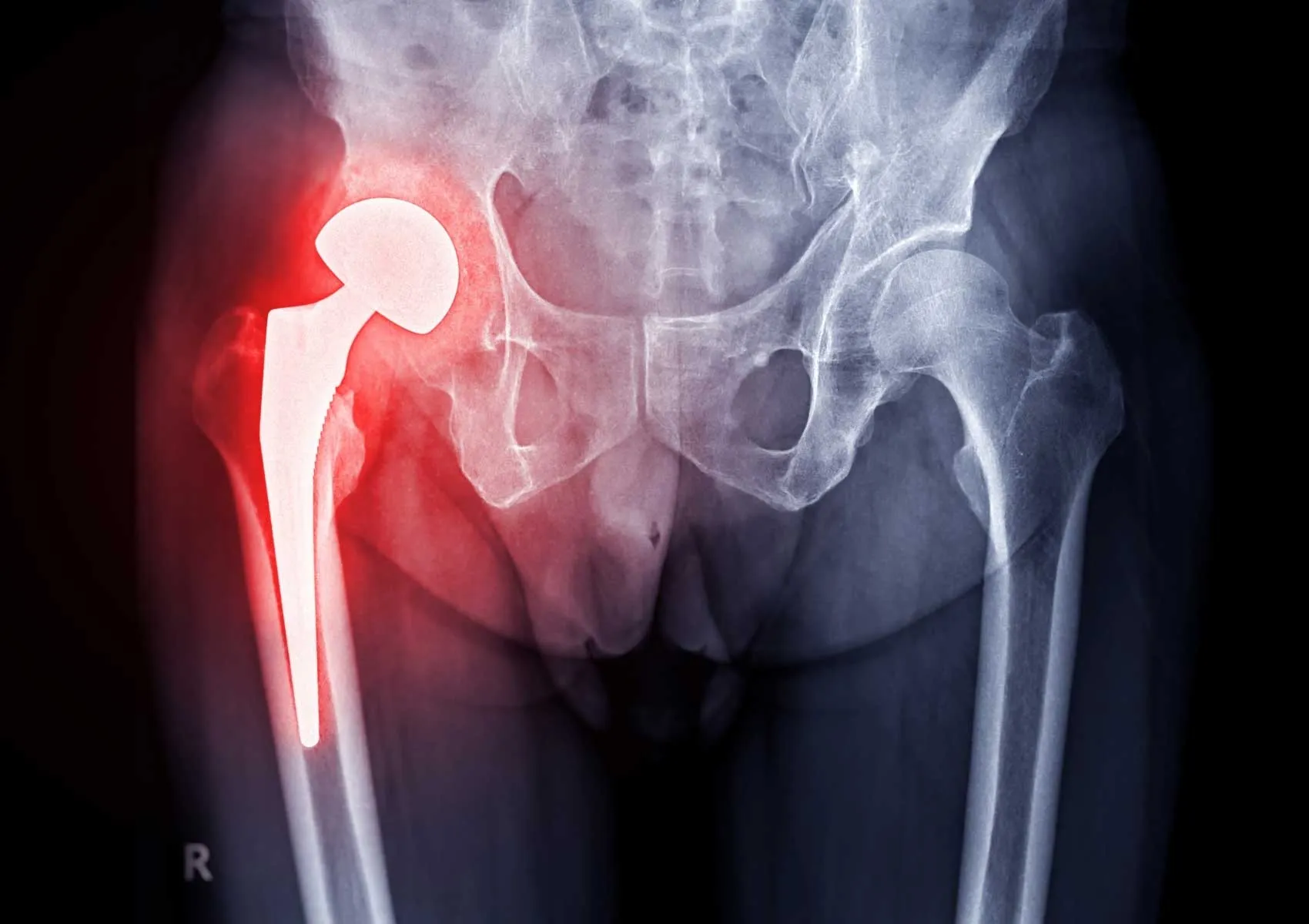
Joint replacement surgeries—particularly for the hip and knee—are highly effective procedures that significantly improve quality of life for patients with advanced joint degeneration. However, like all surgeries, joint arthroplasty carries certain risks. Among the most serious and feared complications is prosthetic joint infection (PJI). Although rare, when it occurs, it can lead to prolonged treatment, additional surgeries, and even loss of the implant.
What Is a Prosthetic Joint Infection?
A prosthetic joint infection occurs when microorganisms, typically bacteria, colonize the area around the implanted joint. These infections may develop shortly after surgery or even years later.
Commonly affected joints include:
- Knee prosthesis (total knee arthroplasty)
- Hip prosthesis (total hip arthroplasty)
- Shoulder and elbow prostheses (less common)
Typical pathogens:
- Staphylococcus aureus
- Coagulase-negative staphylococci
- Pseudomonas aeruginosa
- Enterococcus species
Risk Factors for Joint Infection
Several patient-related and surgical factors can influence the risk of developing a prosthetic infection.
1. Patient-Related Risk Factors
- Diabetes mellitus
- Obesity
- Weakened immune system (immunosuppression)
- Smoking
- Autoimmune diseases (e.g., rheumatoid arthritis)
- Previous joint infections
- Advanced age
2. Surgical Risk Factors
- Prolonged operation time
- Suboptimal sterility or surgical technique
- Excessive blood loss
- Revision (repeat) surgeries
- High-volume hospital environments with increased exposure
When Do Infections Occur?
Based on timing, prosthetic joint infections are categorized into:
- Early infections: Within 3 months post-surgery; usually more aggressive
- Delayed infections: Between 3 months and 2 years post-op; symptoms may be subtle
- Late infections: After 2 years; often spread through the bloodstream from another infection site
Signs and Symptoms
While some infections are obvious, others may be more difficult to detect. Common symptoms include:
- Redness, warmth, or swelling around the surgical site
- Persistent wound drainage
- New or increasing joint pain
- Fever, chills, or fatigue
- Decreased joint function or stiffness
- Radiologic signs like peri-prosthetic bone loss
Diagnosis of Prosthetic Joint Infection
Diagnosis requires a thorough evaluation combining clinical, laboratory, and imaging findings.
- Blood tests: Elevated CRP, ESR, or white blood cell count
- Joint aspiration: Synovial fluid culture and analysis
- Imaging: X-rays, MRI, nuclear scans, or PET
- Tissue biopsy: When needed, for microbial and histopathological analysis
Treatment Options
Management depends on the type of infection, the pathogen involved, and how long the infection has been present.
1. Antibiotic Therapy
Effective in early, mild cases if started promptly.
2. DAIR Procedure (Debridement, Antibiotics, and Implant Retention)
Used for early infections without removing the implant.
3. Revision Surgery
For chronic or severe infections. Two approaches:
- One-stage revision: Infected implant is removed and replaced in the same surgery.
- Two-stage revision: Implant is removed, temporary antibiotic spacer placed, and new implant is inserted after infection control.
Preventing Joint Infections
Both the surgeon and the patient play a role in minimizing infection risk.
Preoperative Measures
- Control of diabetes and chronic diseases
- Smoking cessation
- Weight management if obese
Intraoperative Measures
- Strict aseptic technique
- Prophylactic antibiotics
- Minimizing surgical time
Postoperative Measures
- Proper wound care
- Monitoring for signs of infection
- Antibiotic prophylaxis before dental or urological procedures (if recommended)
FAQ
-
When does prosthetic joint infection usually occur?
Most infections occur within 3 months post-op, but late infections can develop even years later.
-
Is it possible to treat a joint infection without removing the prosthesis?
In early-stage infections, antibiotics and surgical debridement may be sufficient.
-
Can a prosthetic infection be fatal?
Rarely, if untreated, it can lead to sepsis—a life-threatening condition.
-
Can I get another prosthesis after an infection?
Yes, revision surgery is possible after proper infection control.
-
Can dental work cause a prosthetic infection?
Yes. Bacteria from dental procedures may enter the bloodstream and affect the implant. Prophylactic antibiotics may be advised.