New Approaches in Joint Protective Treatments
Newly developed methods in joint protective treatments aim to delay surgical interventions particularly in hip and knee joint diseases, enhancing quality of life. This article explores the latest techniques and scientific advancements in detail.
Joint protective treatments are designed to preserve joint function and improve quality of life, especially before advanced-stage osteoarthritis and degenerative changes occur in hip and knee joint diseases. In recent years, various innovations have emerged in this field, developing modern techniques that reduce the need for surgical interventions and accelerate recovery processes. This article examines the leading new methods in joint protective treatments in light of current advancements in orthopedics and traumatology.
Advancements in Arthroscopic Techniques
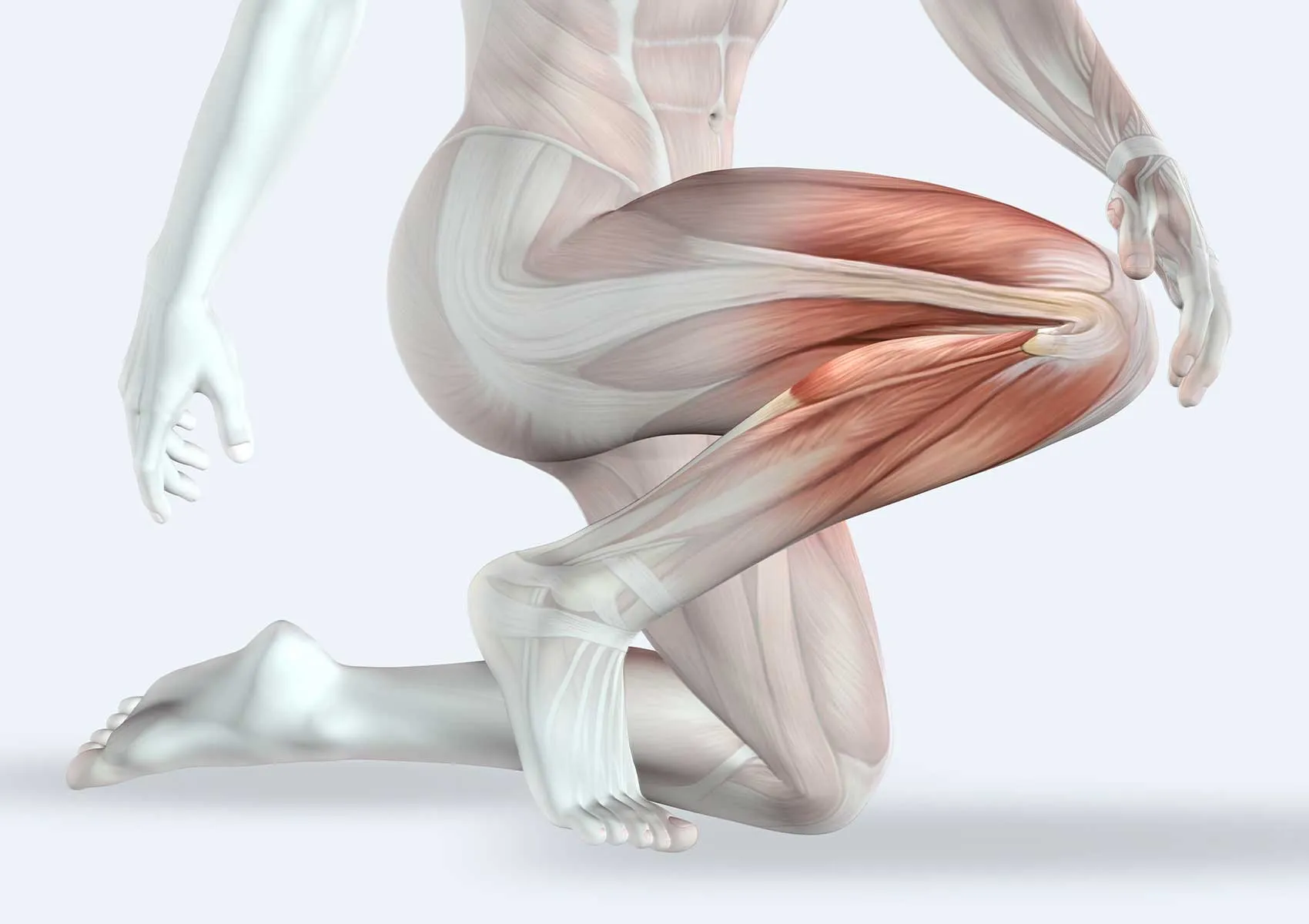
Arthroscopy continues to be the gold standard as a minimally invasive surgical method for the diagnosis and treatment of intra-articular pathologies. Thanks to next-generation arthroscopic equipment and high-resolution camera technology, visualization has significantly improved, enabling precise interventions with smaller incisions. Arthroscopic repairs especially for meniscus tears, cartilage damage, anterior cruciate ligament (ACL), and labrum tears facilitate patients’ early return to daily activities.
Regenerative Approaches in Cartilage Repair
Due to the limited self-renewal capacity of cartilage tissue, regenerative medicine is employed in treating cartilage damage. Stem cell therapies (such as mesenchymal stem cells), growth factors, and platelet-rich plasma (PRP) injections stimulate cartilage regeneration and help preserve functionality in the injured area. Newly developed biomaterials and synthetic scaffold structures also provide support in the cellular growth environment.
Biomaterials and Tissue Engineering
Biomaterials used in joint protective treatments serve supportive functions in cartilage damage and meniscus repairs. These scaffolding structures, composed of natural and synthetic materials, combined with tissue engineering techniques, facilitate cell adhesion, proliferation, and differentiation. The application of these methods in hip and knee joints shortens postoperative healing times and prolongs preservation of joint functions.
Gene Therapies and Molecular-Level Interventions
Innovative molecular-level approaches in joint disease treatment have emerged recently through gene therapy. Targeting and modifying genes that prevent or slow cartilage degradation can halt the progression of degenerative changes and enhance the effectiveness of joint protective treatments. Although still under research, these methods are expected to be integrated into daily clinical practice in the near future.
Early Intervention in Hip and Knee Osteoarthritis
Structural precursors such as acetabular dysplasia and femoroacetabular impingement should be identified early to direct patients toward protective treatments. Arthroscopic debridement, osteotomy, and localized regenerative applications contribute to preserving joint surfaces in these patients. In the knee, early arthroscopic repair of meniscus and cartilage damage associated with anterior cruciate ligament injuries reduces the future need for prosthetic surgery.
Protective Approaches in Sports Injuries
Early protective treatments for hip and knee injuries common among athletes are crucial for maintaining performance levels. Arthroscopic reconstruction techniques that restore anatomical integrity in anterior cruciate ligament repairs reestablish joint stability and limit the development of osteoarthritis. Cartilage and meniscus protective interventions also accelerate return to sports activities.
Protective Strategies in Prosthetic Surgery
When joint protective treatments are not possible and advanced osteoarthritis develops, joint prosthetic surgery becomes necessary. However, current advancements in surgical methods and implant materials aim to extend prosthetic life expectancy and reduce surgical frequency. Minimally invasive approaches, bioactive coatings, and customized implants decrease complications and delay repeat surgeries, enabling patients to live longer with joint function close to natural.
Importance and Future of Joint Protective Treatments
Joint protective treatments not only reduce patient pain but also preserve joint function long-term, minimizing the need for surgical interventions. Multidisciplinary approaches, biotechnological advancements, and personalized treatment plans increase success in this field. In the future, genetic analyses and artificial intelligence-supported diagnostic methods will enable more effective, early, and individualized treatments.
FAQ
-
What is joint protective treatment and who is it suitable for?
Joint protective treatment refers to non-surgical or minimally invasive methods aimed at preserving joint health. It is generally suitable for patients in the early stages of osteoarthritis, those with meniscus or cartilage damage, or anterior cruciate ligament injuries.
-
Why is arthroscopic surgery preferred?
Arthroscopic surgery is preferred because it is minimally invasive, shortens recovery time, reduces pain, and allows comprehensive treatment of intra-articular pathologies. It is especially effective for meniscus, cartilage, anterior cruciate ligament, and labrum tears.
-
How are stem cell therapies used in joint protective treatments?
Stem cell therapies are regenerative applications that promote the renewal of damaged cartilage tissue and reduce inflammation. They can be administered following arthroscopic procedures or by injection.
-
What advantages do new-generation biomaterials provide?
Biomaterials support cellular growth, adapt to the biomechanical properties of the tissue, and increase surgical success rates. This enhances the effectiveness of cartilage and meniscus repairs and shortens healing times.
-
When is joint replacement surgery inevitable?
Joint replacement surgery is recommended in advanced osteoarthritis when conservative and protective treatments are insufficient and severe pain and functional loss limit daily activities.