Cartilage Damage in the Knee: Why Early Intervention Matters
A Silent Threat to Joint Health
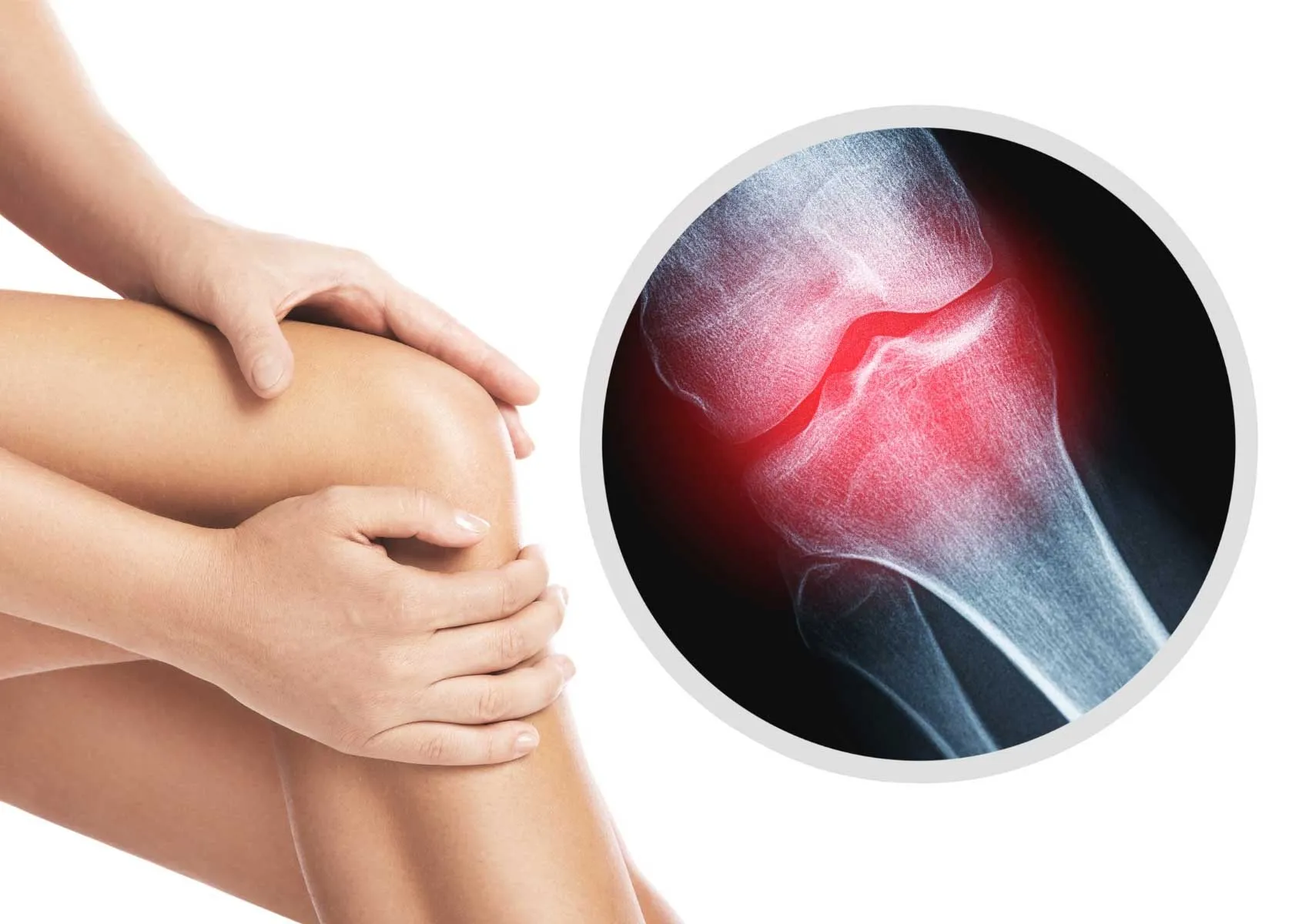
The knee joint is one of the most complex and heavily used joints in the human body. It plays a crucial role in bearing body weight, enabling movement, and supporting athletic performance. At the heart of this functionality lies the articular cartilage—a smooth, elastic, and shock-absorbing tissue that covers the ends of bones within the joint.
When this tissue is damaged, it can silently initiate a progressive cycle of degeneration that may lead to chronic pain, restricted mobility, and, eventually, joint failure. Cartilage injuries in the knee, particularly in their early stages, are often subtle and easy to overlook. However, delaying treatment can result in serious long-term consequences.
In this article, we explore the structure of cartilage, how damage occurs, why early intervention is critical, and the available treatment options.
What Is Articular Cartilage and Why Is It Important?
Articular cartilage is a specialized connective tissue that covers the ends of bones where they meet to form a joint. It allows smooth, frictionless motion and absorbs impact during activities like walking, running, and jumping. One of its key features is that it is avascular—meaning it lacks blood vessels. As a result, it has very limited self-healing capacity.
Even minor injuries to the cartilage can expand over time, affecting the entire joint surface. When untreated, this damage extends to surrounding structures such as the meniscus, ligaments, subchondral bone, and the joint capsule, ultimately leading to osteoarthritis.
How Does Cartilage Damage Occur?
Cartilage injuries can occur due to a single traumatic event (e.g., a fall or twist) or through repetitive microtrauma over time. Aging also plays a significant role, as cartilage naturally loses elasticity and thickness with wear.
Common causes include:
- Sports injuries and twisting movements
- Ligament injuries (especially ACL tears)
- Meniscal tears that alter load distribution
- Chronic overuse or repetitive stress
- Obesity and prolonged weight-bearing
- Congenital or structural abnormalities
- Age-related degenerative changes
In younger, active individuals, cartilage injuries are more likely to be traumatic, while in older adults, they are typically degenerative in nature.
What Are the Symptoms?
Cartilage damage often presents subtly in the early stages, which makes diagnosis challenging. However, certain warning signs should raise suspicion:
- Localized pain in the front or inside of the knee
- Discomfort or aching after prolonged standing or walking
- Pain while climbing stairs or squatting
- Clicking, grinding, or catching sensations
- Reduced ability to fully bend or extend the knee
- Swelling or stiffness after activity
As the condition progresses, the pain becomes more persistent and may limit daily activities, leading to muscle weakness and reduced function.
Why Is Early Intervention So Important?
Because cartilage has minimal regenerative capacity, early detection and treatment can prevent irreversible joint degeneration. Timely intervention can also reduce the likelihood of needing more invasive procedures, such as joint replacement, later in life.
Benefits of early treatment include:
- Preventing progression of minor injuries
- Preserving natural joint structure and function
- Reducing or eliminating pain
- Postponing or avoiding prosthetic surgery
- Supporting quicker return to activity or sport
Delaying treatment often leads to worsening damage, involvement of multiple joint components, and more complex and less predictable treatment outcomes.
Treatment Options
Treatment depends on the size, location, and depth of the cartilage defect, as well as the patient’s age, activity level, and overall joint condition.
Non-surgical (conservative) treatments:
- Physical therapy and muscle strengthening
- Intra-articular injections (PRP, hyaluronic acid, stem cells)
- Weight management and activity modification
- Anti-inflammatory medications
- Transition to low-impact sports (e.g., cycling, swimming)
Surgical options:
- Arthroscopic debridement: Smoothing the damaged area to reduce irritation
- Microfracture: Stimulating new cartilage growth by creating small holes in the bone
- Mosaicplasty (osteochondral grafting): Transferring healthy cartilage from another area
- Autologous Chondrocyte Implantation (ACI/MACI): Harvesting, culturing, and reimplanting the patient’s own cartilage cells
When applied early, these methods can produce excellent outcomes and help patients maintain an active lifestyle without the need for joint replacement.
FAQ
-
Can cartilage heal on its own?
No. Articular cartilage lacks blood supply and has very limited ability to regenerate without medical intervention.
-
Does every cartilage injury require surgery?
Not always. Small and early-stage injuries may respond well to non-surgical treatment.
-
How do I know if cartilage damage is getting worse?
Persistent pain, stiffness, and reduced range of motion despite rest suggest progression.
-
Are cartilage repair procedures permanent?
They can offer long-term relief, especially when applied early, but outcomes vary depending on the extent of the damage.
-
Can I continue exercising with cartilage damage?
Yes, but with modifications. Low-impact activities are encouraged, while high-impact exercises should be avoided or limited.