Is PRP Treatment Effective for Hip Joint Problems?
PRP (Platelet Rich Plasma) treatment's effectiveness in hip joint problems is attracting increasing attention. This article discusses what PRP treatment is, its applications in hip joint issues, supporting scientific data, and the treatment process.
The hip joint is one of the largest weight-bearing joints in the body and plays a critical role in mobility and quality of life. Aging, injuries, and chronic diseases can cause pain and functional loss in the hip joint. Recently, PRP treatment (Platelet Rich Plasma), one of the biological therapies emerging in orthopedics alongside stem cell therapies, has gained prominence for addressing hip joint problems.
What Is PRP Treatment?
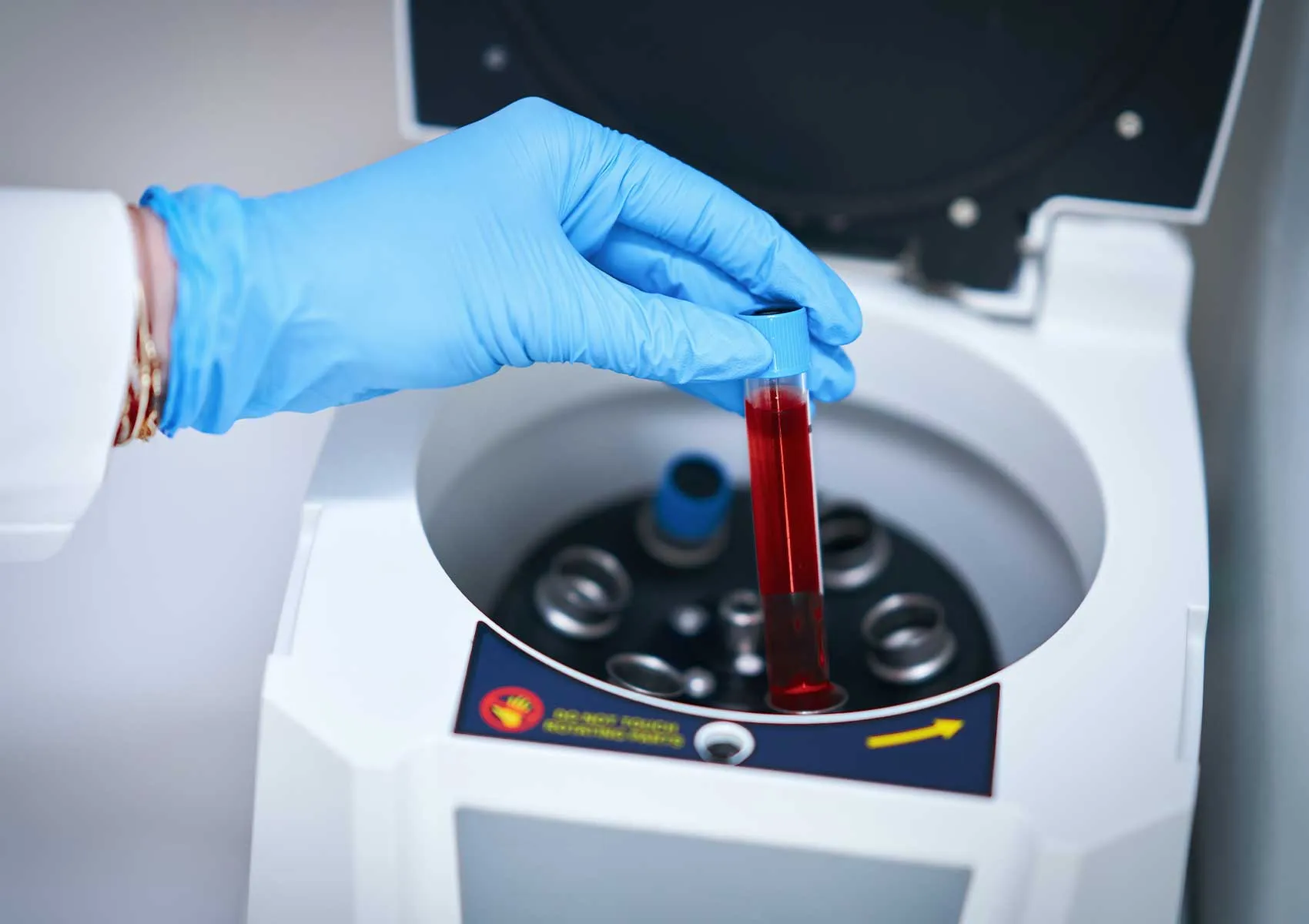
PRP treatment involves drawing blood from the patient and enhancing its platelet concentration through special methods before injecting it into the joint or tissue. Platelets are rich in growth factors that accelerate tissue repair and reduce inflammation. This non-surgical biological treatment supports the natural healing process.
Use of PRP in Hip Joint Problems
Common hip joint issues include osteoarthritis, femoroacetabular impingement, labral tears, and cartilage damage. Studies indicate that PRP injections can reduce pain and improve function, especially in early to moderate osteoarthritis cases. PRP targets the soft tissues around the hip joint to decrease inflammation and slow cartilage deterioration.
Benefits and Limitations of PRP Treatment
The primary advantages of PRP therapy include its biological and minimally invasive nature, and the very low risk of allergic reactions since it is derived from the patient's own blood. It provides a valuable alternative for patients unsuitable for or unwilling to undergo surgery. However, PRP alone may not be sufficient for advanced osteoarthritis cases, and surgical interventions might be necessary in combination. Additionally, treatment efficacy can vary among individuals.
Scientific Basis for PRP Application in Hip Health
Recent clinical studies show that PRP reduces pain and inflammation while delaying functional decline in the hip joint. For example, patients with early-stage hip osteoarthritis experience significant symptom relief and improved quality of life after PRP injections. Nonetheless, there is no standardized consensus on PRP application protocols and dosages in the literature, necessitating individualized treatment plans based on specialist evaluation and patient conditions.
Who Is Suitable for PRP Treatment?
PRP is typically recommended for early-stage hip osteoarthritis, femoroacetabular impingement, and labral tears involving soft tissue and cartilage issues within the joint. It may be inadequate alone for severe cartilage loss, advanced osteoarthritis, or bone degeneration. Structural deformities often require arthroscopic or open surgery. PRP can also aid recovery from sports injuries by accelerating healing.
How Is PRP Treatment Applied?
The procedure entails drawing a small amount of blood from the patient, processing it in specialized centrifuges to isolate plasma rich in platelets. The obtained PRP is then injected into the hip joint under sterile conditions, usually guided by ultrasound or other imaging techniques. Treatment commonly involves multiple sessions spaced at set intervals. Patients can typically resume daily activities shortly after each session.
Side Effects and Precautions
Since PRP is autologous—derived from the patient’s own blood—the risk of allergic reactions is very low. Temporary discomfort, tenderness, or mild inflammation may occur at the injection site. Infection risk is minimal but strict sterilization protocols must be followed. Rest and physical therapy as advised by the physician before and after treatment can complement recovery.
FAQ
-
How effective is PRP treatment for hip osteoarthritis?
PRP can reduce pain and improve function in early to moderate hip osteoarthritis but may be insufficient alone in advanced stages where surgery might be necessary.
-
Is PRP treatment painless?
Local anesthesia is usually applied before the injection, making the procedure minimally painful. Mild pain may occur afterward but typically subsides quickly.
-
When can I return to sports after PRP treatment?
Rest and physical therapy schedules are determined by the doctor. Light activities can usually begin within 1-2 weeks depending on pain levels.
-
Is PRP treatment a permanent solution?
PRP can delay damage progression and ease symptoms but does not fully regenerate cartilage. It is often combined with other treatments.
-
Who is not suitable for PRP treatment?
Patients with blood disorders, bleeding problems, infections, or advanced joint deformities may not be candidates for PRP. Thorough evaluation by a physician is essential.